Intraoperative Neurophysiological Monitoring Of Acoustic Neuroma
Hearing nerve (sheath) tumors, also known as vestibular schwannomas, are the most common benign tumors found in the cerebellopontine angle (CPA). These tumors typically arise from the vestibular portion of the auditory nerve and are usually unilateral, with bilateral occurrences being rare. As these tumors grow slowly, they can exert pressure on nearby cranial nerves and the cerebellum, potentially displacing the brainstem and compressing the cerebral aqueduct, leading to serious complications such as cerebellar tonsillar herniation.
At NCC, we have been dedicated to advancing neurophysiological technology for over 27 years, providing cutting-edge solutions that facilitate safe surgical practices while enhancing patient care. Our commitment to innovation ensures that we continue to lead in developing high-end electrophysiological equipment tailored for neurosurgery applications.
As the tumor progresses, patients may experience severe symptoms that can threaten their lives. The primary goal of surgical intervention for hearing nerve tumors is to safely achieve total tumor removal while preserving facial nerve function and minimizing significant neurological sequelae such as postoperative coma, hemiplegia, or facial nerve paralysis. Additionally, for patients with functional hearing, efforts should be made to preserve their hearing.
The Role of Intraoperative Neurophysiological Monitoring
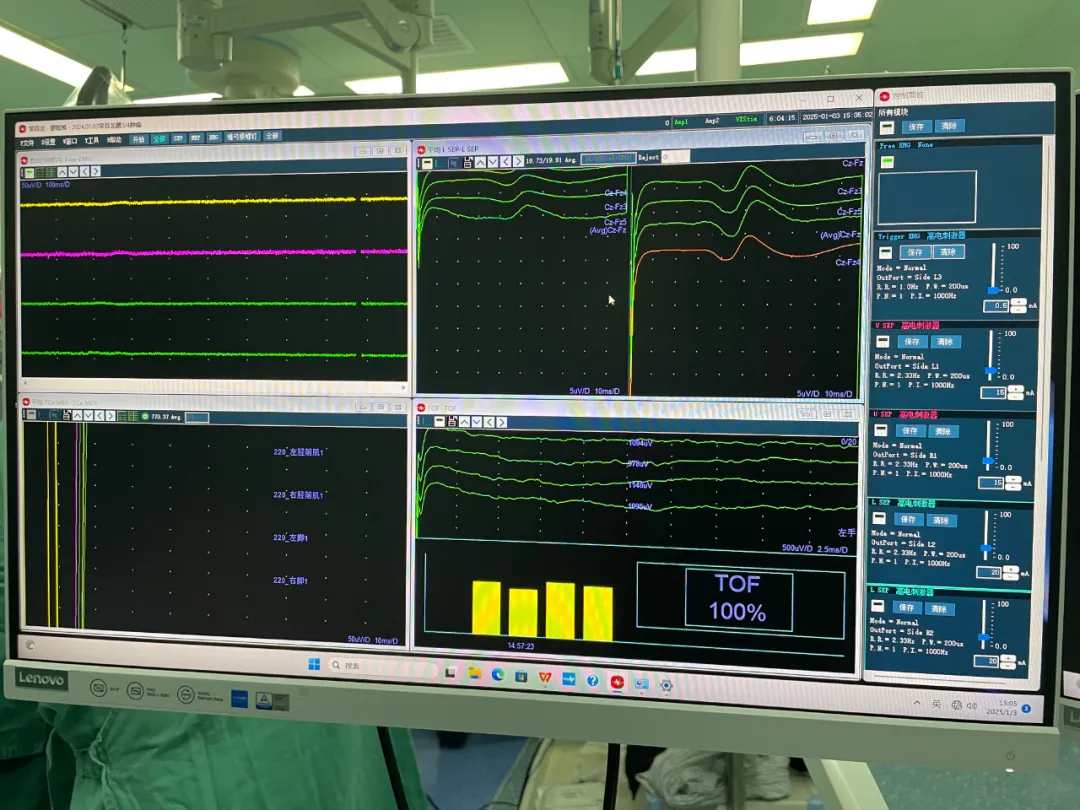
Intraoperative neurophysiological monitoring (IONM) plays a crucial role during hearing nerve tumor surgeries. It helps in early detection of potential nerve damage and minimizes postoperative complications. Here are some key monitoring parameters used during surgery:
1. Free Electromyography (Free EMG)
Free EMG is used to monitor the traction responses of cranial nerves such as the trigeminal nerve (V), facial nerve (VII), vagus nerve (X), accessory nerve (XI), and hypoglossal nerve (XII). This real-time feedback allows surgeons to assess nerve integrity during tumor manipulation.
2. Triggered Electromyography (Trigger EMG)
Triggered EMG involves electrical stimulation of cranial nerves to help locate and identify their pathways. This technique is essential for avoiding inadvertent damage to critical structures during surgery.
3. Facial Motor Evoked Potentials (Facile MEP)
Facile MEPs are recorded to evaluate facial nerve function during surgery. Monitoring includes specific muscle groups such as the masseter, frontalis, orbicularis oculi, orbicularis oris, mentalis, cricothyroid muscle, and trapezius muscle. Stimulation is performed at designated sites to ensure accurate assessment.
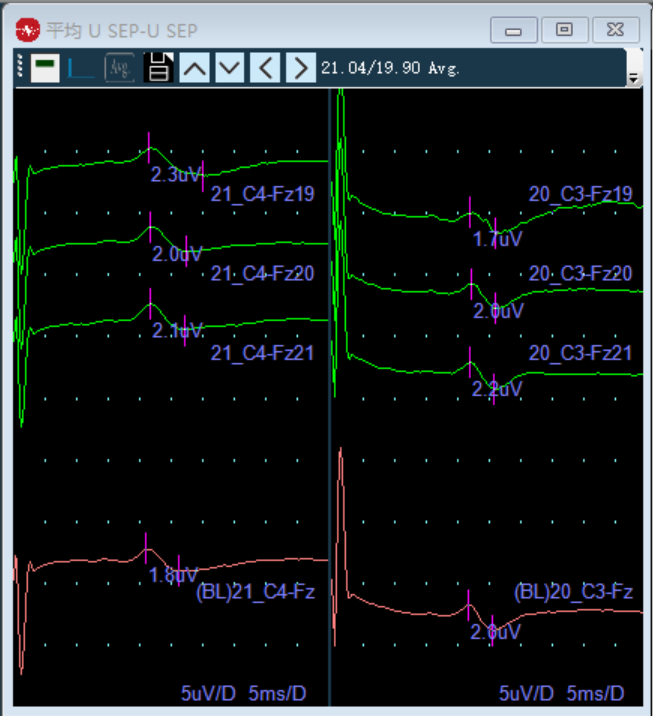
4. Brainstem Auditory Evoked Potentials (BAEP)
BAEP monitoring assesses the function of the auditory nerve and brainstem. It is crucial for protecting auditory function during surgery, especially when dealing with tumors that may affect hearing.
5. Somatosensory Evoked Potentials (SSEP)
SSEP monitoring provides information about sensory pathways in the upper limbs and helps assess brainstem function during surgical procedures.
Monitoring Protocols and Alerts
During surgery, specific monitoring protocols are established:
1. Pre- and Post-Tumor Resection Monitoring: SSEP, BAEP, and Facile MEP should be recorded before tumor resection begins and continuously monitored for 2-3 minutes after resection.
2. EMG Stimulation: A square wave pulse with a duration of 0.2 ms at a rate of 4-6 times per second is used for EMG stimulation. Initial stimulation strength starts at 0.2 mA.
3. Data Recording: Accurate measurement of latency and amplitude changes is critical for assessing potential neurological compromise.
Alert Standards
The following alert standards are established for intraoperative monitoring:
1. Free EMG: Any significant traction response should alert the surgical team.
2. BAEP: A latency increase of 10% or amplitude decrease below 50% indicates potential issues.
3. Facile MEP: Similar criteria apply as with BAEP monitoring.
4. SSEP: A latency increase or amplitude decrease indicates possible sensory pathway compromise.
Surgical Considerations
When performing surgery in the CPA region, several important considerations must be kept in mind:
1. Careful Dissection: During tumor dissection from the inner wall, only cut branches supplying blood to the tumor; avoid damaging major vessels that supply blood to the brainstem.
2. Preservation of Nerve Integrity: Utilize microscopic surgical instruments carefully to preserve facial and auditory nerves while maintaining anatomical relationships.
3. Complete Tumor Resection: Aim for total resection while allowing sufficient space for brainstem repositioning to minimize intraoperative bleeding and relieve intracranial pressure.
4. Monitoring Hemodynamics: In case of significant bleeding during surgery, timely transfusion or fluid administration is crucial to prevent shock.
5. Postoperative Care: Monitor patients closely for any signs of neurological deficits or complications following surgery.
Conclusion
The surgical management of hearing nerve tumors presents unique challenges due to their location and potential impact on critical neural structures. Intraoperative neurophysiological monitoring is essential for minimizing risks associated with these complex procedures. By employing advanced techniques like Free EMG, Trigger EMG, BAEP, SSEP, and Facile MEP monitoring, surgeons can enhance patient safety and improve outcomes.
If you’re interested in learning more about our products or how we can support your clinical needs in neurosurgery or other medical fields, please contact us today! Together, we can work towards improving surgical outcomes and enhancing patient safety through advanced technology solutions.

 中文
中文 Arabic
Arabic Spanish
Spanish Hindi
Hindi French
French Indonesian
Indonesian Portuguese
Portuguese Persian
Persian Russian
Russian Korean
Korean German
German Vietnamese
Vietnamese Turkish
Turkish