Precisely Disarming the "Nerve Bomb": Intraoperative Neurophysiological Monitoring Guides Complex Malignant Melanoma Resection
On the eve of the New Year, Mr. Zhang (a pseudonym), a 48-year-old patient, was urgently admitted to our hospital due to sudden severe headache accompanied by convulsions. The imaging results were shocking: the patient, still in his forties, had large space-occupying lesions in multiple segments of the brain, thoracic vertebrae, and lumbar-sacral vertebrae. The lesions were surrounded by severe edema, with brain tissue compression and involvement of the conus medullaris and cauda equina, leading to symptoms of headache, convulsions, progressive weakness in both lower limbs, and urinary and fecal dysfunction.
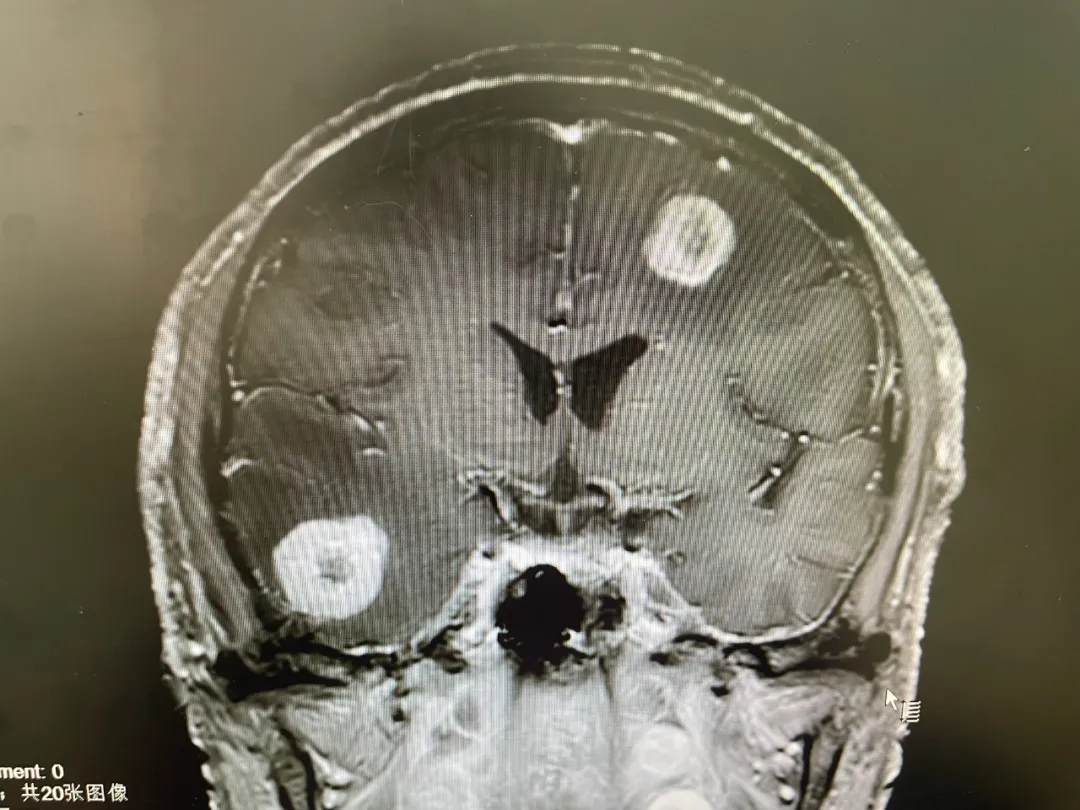

Preoperative Imaging
Moreover, the tumor was highly suspected to be malignant. As the sole breadwinner of the family, the family strongly requested that the surgery should maximize tumor resection to obtain pathological results while ensuring no neurological damage.
Multidisciplinary Consultation: Formulating a Precise "Demining" Plan
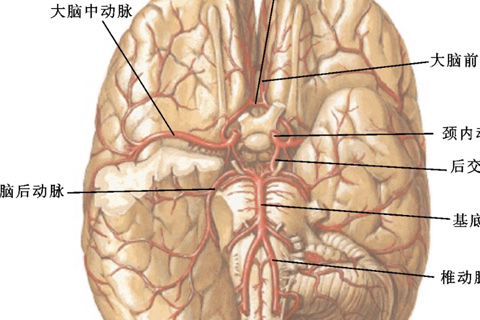
Faced with this extremely complex case, the neurosurgery team quickly initiated a multidisciplinary consultation (MDT). The three-dimensional reconstruction results showed that the tumor had a wide range of invasion, involving the motor cortex and lumbosacral nerve roots. Traditional surgical methods would easily lead to permanent nerve damage. After in-depth discussion, the team innovatively proposed a "three-step" strategy:
1. Stereotactic Precision Localization
Using the ROSA robot to construct a spatial model of the lesion and plan the optimal surgical approach to minimize surgical trauma to the patient.
2. Intraoperative Neurophysiological Monitoring Throughout the Procedure
Adopting SSEP + MEP combined monitoring with dual early warning thresholds (amplitude decrease > 50% or latency prolongation > 10%), to clearly identify the location of nerves and minimize nerve interference.
3. Staged Decompression Surgery
Prioritize the removal of life-threatening intracranial lesions, followed by treatment of spinal cord lesions to improve the patient's quality of life and extend healthy living time, reducing the risk of paralysis and urinary/fecal incontinence.
Intraoperative "Bomb Disarming": Millimeter-Level Operations to Protect Nerve Function
On the day of the surgery, with the anesthesiology team precisely controlling the depth of anesthesia, the neurophysiological monitor was capturing every fluctuation of nerve signals in real-time. When removing the tumor in the motor cortex, the MEP waveform attenuation triggered an early warning, immediately alerting the chief surgeon to maximize tumor resection while preserving nerve function. After a 9-hour operation, the team successfully performed subtotal resection of the intracranial lesion and sacral canal tumor, with the critical nerve tracts fully preserved.

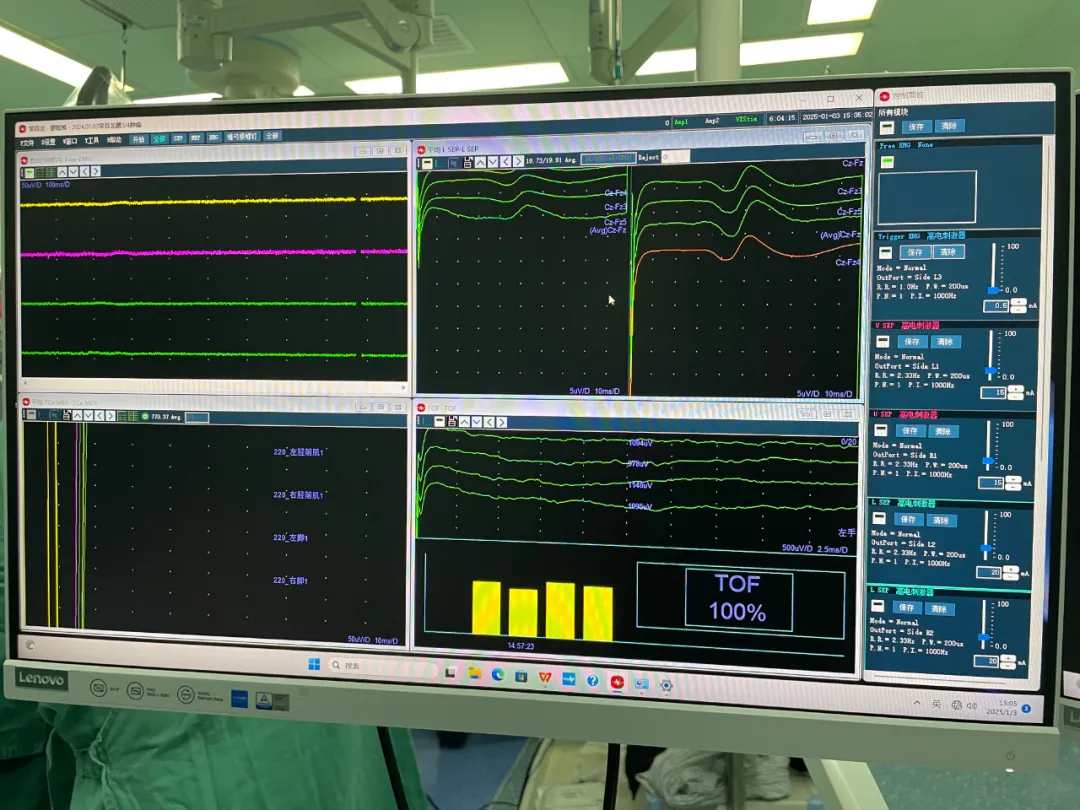
During the Surgery
The day after the surgery, the patient's limb movement and urinary/fecal functions were not worsened compared to preoperatively. The postoperative pathology report confirmed malignant melanoma, consistent with the characteristics of systemic metastasis.
Extended Reading
[Intraoperative Neurophysiological Monitoring] acts like a surgical navigation system. By monitoring bioelectrical signals such as somatosensory evoked potentials (SSEP) and motor evoked potentials (MEP), it can issue a warning 0.5-2 seconds before nerve damage occurs, transforming nerve function protection from "experience-based judgment" to "quantitative safeguarding."
[Nervous System Melanoma] These "neurological stealthers" have a neurotropic nature, with a 5-year survival rate of less than 20%. The latest "CNS Melanoma Diagnosis and Treatment Guidelines" emphasize that the scope of resection should be dynamically balanced with functional protection, and multimodal intraoperative neurophysiological monitoring provides crucial technical support for such surgeries.
Postoperative Insights
This successful case demonstrates that for complex nerve tumors, precise surgical techniques based on multimodal intraoperative neurophysiological monitoring can significantly improve the rate of complete resection and functional preservation, offering improved quality of life for more end-stage patients.

 中文
中文 Arabic
Arabic Spanish
Spanish Hindi
Hindi French
French Indonesian
Indonesian Portuguese
Portuguese Persian
Persian Russian
Russian Korean
Korean German
German Vietnamese
Vietnamese Turkish
Turkish